Imagine a world where your medical records are stored on floppy disks, and your doctor has to use a rotary phone to coordinate your care. Sounds archaic, doesn’t it? Yet, this is close to reality for many healthcare providers, with a startling 73% still relying on legacy software.
The consequences of holding on to these outdated systems are severe. The U.S. federal government spends a staggering $337 million annually to keep ten of its legacy systems operational. But the real cost goes beyond just money.
Legacy systems make it harder for healthcare providers to deliver secure, reliable, and scalable services. This may compromise patient care and risk exposing sensitive data.
Despite these challenges, the global healthcare IT market will become a $728.63 billion entity by 2029. So, modernizing healthcare legacy systems is no longer a luxury; it’s a necessity for providers who want to stay competitive and provide the best possible care.
This comprehensive guide will explain the needs, challenges, approaches, and step-by-step process of modernizing legacy systems in healthcare.
What is a legacy system in healthcare?
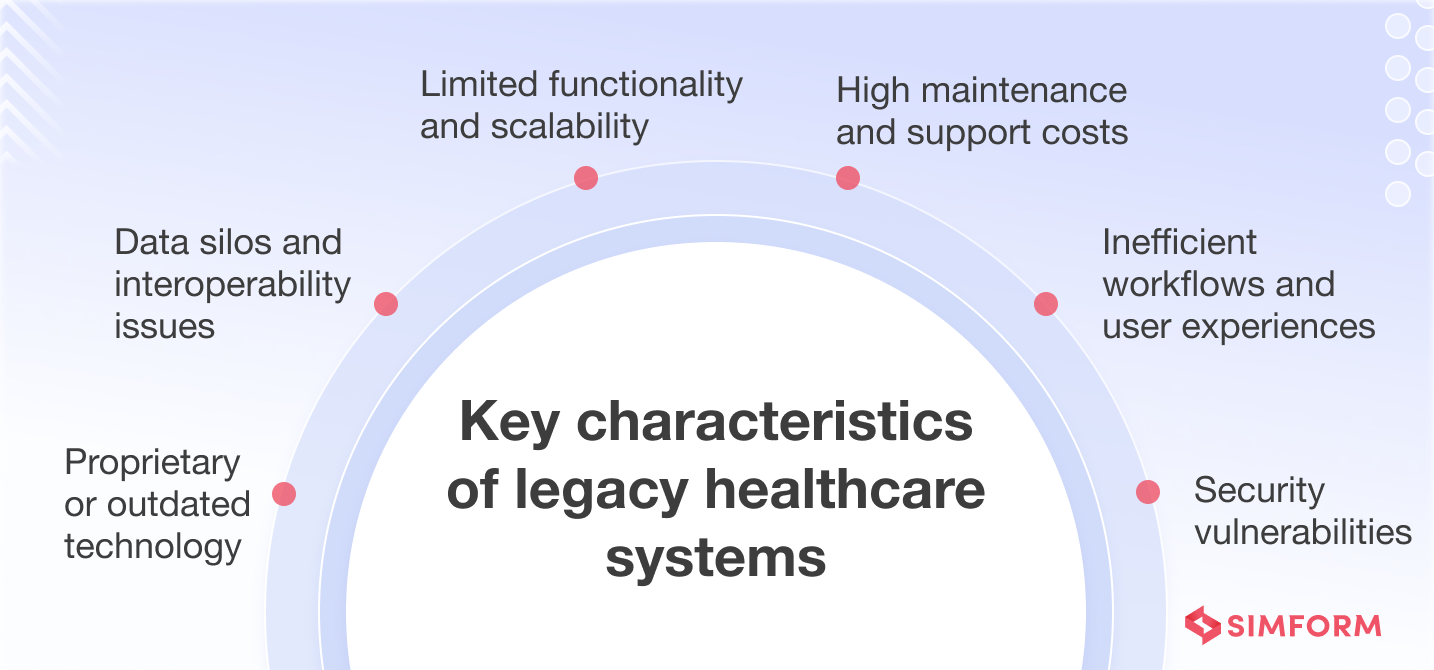
A legacy system in healthcare refers to an outdated software application or technology platform that a healthcare organization continues to use despite its limitations and the availability of newer, more advanced solutions. These systems often have been in place for many years and are deeply integrated into the organization’s workflows and processes.
Although they may still function, legacy systems in healthcare can pose challenges such as limited interoperability with newer technologies, difficulty in maintaining and updating, and potential security vulnerabilities.
Types of legacy healthcare IT systems
Legacy systems come in various forms, each with its own set of challenges and implications for patient care and organizational efficiency. The following are the main types of legacy systems in healthcare settings:
#1. Electronic Health Record (EHR) Systems
Early EHR systems focused on basic patient record keeping and may lack modern functionalities, interoperability, and user interfaces.
#2. Hospital Information Systems (HIS)
Legacy HIS systems that manage administrative, financial, and clinical hospital operations may struggle with interoperability, real-time data access, and reporting capabilities.
#3. Laboratory Information Systems (LIS)
Legacy LIS systems that manage laboratory data and workflows may face issues with data standardization and integration with newer diagnostic technologies.
#4. Picture Archiving and Communication Systems (PACS)
Outdated PACS for medical image storage and retrieval may have limited storage capacity, slow retrieval speeds, and compatibility issues with new imaging modalities.
#5. Radiology Information Systems (RIS)
Older RIS systems that monitor radiology workflows, scheduling, and billing may lack capabilities like automatic appointment scheduling. Legacy RIS may also lack integration with other systems, leading to duplicate data entry, billing errors, and inefficient resource utilization.
#6. Telemedicine Systems
Legacy telemedicine systems in healthcare communications infrastructure may need upgrading to provide secure communication and effective telehealth services.
#7. Claims Processing Systems
Legacy claims processing systems that manage billing and reimbursement between providers and payers may struggle with modern billing rules and regulatory changes
#8. Patient Engagement Systems
Patient engagement systems facilitate communication, education, and self-management tools for patients. When these systems become outdated, they may lack user-friendly interfaces, mobile compatibility, and integration with other healthcare IT systems. This can lead to poor patient engagement, lower adherence rates, and suboptimal health outcomes.
To ensure the delivery of high-quality, efficient healthcare services, organizations must carefully weigh the costs and benefits of maintaining these legacy systems against the potential value of modernization initiatives.
Maintaining vs. modernizing healthcare systems
Maintaining vs. modernizing healthcare systems is a crucial decision that requires careful consideration of your organization’s needs and resources. While upgrading may seem like an obvious choice, many organizations choose to maintain legacy systems for various reasons.
Advantages of running existing legacy healthcare systems:
- Cost-effective if current systems function well
- Minimal training and disruption due to staff familiarity
- Better compatibility with existing systems and applications
Advantages of modernizing legacy healthcare systems:
- Improved efficiency through advanced technologies that streamline workflows and enhance interoperability
- Sophisticated security features to protect patient data and ensure compliance
- Future-proofing for compatibility with emerging technologies and organizational growth
The choice between maintaining or modernizing your legacy healthcare system depends on factors like the age and condition of your existing systems, the availability of resources (financial, technical, and human), and your organization’s long-term goals and priorities.
Despite the benefits of maintaining legacy systems, there comes a point when you cannot avoid modernizing them.
Indicators signalling the need to modernize your healthcare systems
As healthcare technologies continue to evolve at an unprecedented pace, it becomes increasingly crucial for organizations to recognize the telltale signs that your legacy systems are no longer serving your needs effectively.
| Indicator | Description |
| Performance and scalability issues | Noticeable slowdowns, system crashes, or inability to handle increased workload |
| Security and compliance | Frequent breaches, non-compliance with regulations, or outdated security measures |
| UX and adaptability | Poor user experience, difficulty adapting to new system requirements, or outdated interfaces |
| TCO and ROI | The high total cost of ownership and low return on investment compared to newer solutions |
| Limited functionality | The system’s inability to meet current needs, lack of essential features, or outdated capabilities |
| Malfunction and tech incompetence | Frequent system failures, errors, or difficulty maintaining the system |
| Slow and reduced productivity | Decreased efficiency, longer wait times, or difficulty completing tasks point toward system improvements |
| Abandoned or unsupported by the vendor | Lack of vendor support, no updates, or end-of-life announcements for legacy systems |
| Expensive maintenance | High maintenance costs, reliance on outdated components, or difficulty finding maintenance-related support |
| Device dependency | Incompatibility with modern devices, reliance on obsolete hardware, or limited mobility |
| Integration limitations | Difficulty integrating with other systems, lack of interoperability, or reliance on outdated protocols |
| Inefficient workflow | Bottlenecks, redundant processes, or lack of automation highlight the need for system enhancements to streamline workflows |
Risks of not modernizing your legacy healthcare systems
When the above signs are clear, not upgrading your IT systems can have far-reaching consequences for your organization’s operations, patient care, and overall competitiveness.
- Compromised patient safety: Outdated systems increase the risk of medical errors, misdiagnoses, and adverse events due to inaccurate or incomplete patient data, ineffective communication, and lack of interoperability between healthcare providers.
- Data breaches and compliance risks: Legacy systems often lack robust security measures and become vulnerable to cyber threats and data breaches. These breaches can lead to hefty fines and legal repercussions for non-compliance with data privacy regulations.
- Inefficient operations and workflow disruptions: Antiquated systems are prone to downtime, slow performance, and compatibility issues, resulting in workflow disruptions, staff frustration, and decreased productivity.
- Inability to leverage advanced technologies: If you hold on to legacy systems, you risk falling behind in leveraging cutting-edge technologies such as artificial intelligence and machine learning. These technologies can significantly enhance patient outcomes, streamline processes, and reduce healthcare costs.
- Competitive disadvantage: Patients expect seamless experiences and advanced services in an increasingly digital healthcare landscape. Failing to meet these expectations can result in losing patients and revenue to more technologically savvy competitors.
When the signs are clear and you are considering upgrading your systems, make sure to understand each modernization approach thoroughly to make an informed decision.
Top methods for modernizing healthcare systems
Here are the top approaches for modernizing legacy healthcare systems. Each method offers distinct advantages in upgrading healthcare infrastructure.
| Approach | Description | Application |
| Encapsulation | Wrapping legacy systems with modern interfaces or APIs, allowing newer applications to access and integrate with older systems while preserving core functionality | When modernizing the interface or integration capabilities of existing systems without significant changes to the underlying codebase |
| Rehosting (Lift and Shift) |
Migrating an application or system to a new infrastructure or platform, such as moving from on-premises to the cloud, without modifying the application code | When the existing application is stable and performs well but would benefit from running on a modern infrastructure |
| Refactoring | Restructuring and optimizing the existing codebase, improving performance, maintainability, and scalability without altering the external behavior | When the existing codebase is monolithic, tightly coupled, or challenging to maintain, or when you want to reduce tech debt |
| Rebuilding | Rewriting an application or system from scratch, often using modern technologies and architectures, while preserving its core functionality and business logic | When the existing system is too outdated or costly to maintain, or when a complete overhaul is necessary to meet new requirements or take advantage of emerging technologies |
| Replacing | Decommissioning and replacing an existing system with a new, modern solution that better aligns with the organization’s current and future needs | When the system is beyond repair or outdated to modernize, a complete replacement is more cost-effective or better aligned with your long-term goals |
| Rearchitecting | Redesigning the architecture of an existing system, often moving from a monolithic to a microservices, cloud-native, or event-driven architecture to improve scalability, flexibility, and maintainability | When the existing architecture is not suitable for modern requirements, such as cloud-native deployments, high scalability, or rapid feature delivery |
The choice of strategy will depend on factors such as the legacy system’s complexity, criticality, and current performance, as well as the organization’s budget, timeline, and risk tolerance.
Now, let’s go through the intricate steps involved in legacy healthcare system modernization.
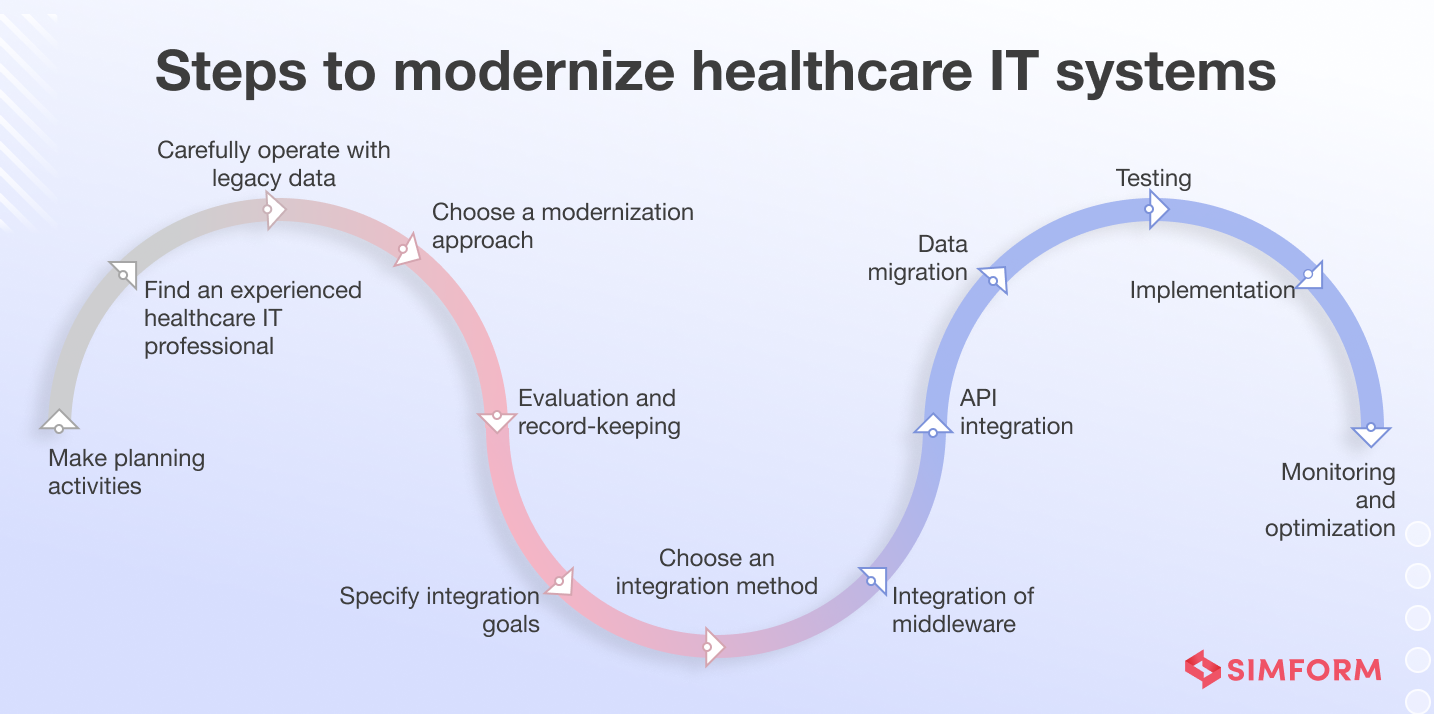
Steps to modernize healthcare IT systems
Modernizing legacy systems is a complex undertaking that requires careful planning, execution, and monitoring to ensure a successful outcome. From initial assessment and planning to implementation, testing, and post-modernization maintenance, here are the essential steps involved in a well-executed healthcare legacy app modernization initiative.
Step 1: Assess the current legacy systems
Begin by conducting a comprehensive IT audit to identify all hardware, software, and systems in use. Analyze their age, performance metrics, compatibility, and security vulnerabilities. We also recommend gathering insights from key stakeholders, including end-users, IT staff, and executive leadership, to understand their needs, concerns, and expectations for the modernized system.
The assessment phase also includes evaluating the total cost of ownership, including software maintenance, support, and downtime costs. This analysis helps organizations understand the financial implications of maintaining legacy systems and the potential long-term benefits of modernization.
Based on the findings, prioritize mission-critical systems that require immediate modernization based on their impact on patient care, operational efficiency, and regulatory compliance. Finally, develop a detailed report outlining the findings, risks, and recommendations for a phased modernization approach.
Step 2: Choose a modernization approach
When modernizing legacy systems in healthcare, consider approaches that prioritize data security, compliance, and seamless integration with existing healthcare workflows.
- Rehosting: Use when you need to quickly migrate the app to the cloud with minimal changes, but it may not address underlying issues or leverage cloud-native features.
- Refactoring: Use when you want to improve the app’s performance and compatibility without significantly altering its architecture.
- Rearchitecting: Use when you need to align the app’s architecture with modern best practices for better modularity and scalability, but it requires more effort and resources compared to rehosting or refactoring.
- Rebuilding: Use when the legacy app is no longer viable, and you want to create a new, modern app, but it comes with higher costs and longer timelines.
- Replacing: Use when the legacy app no longer serves its purpose, and you want to adopt a new solution that better meets requirements, but ensure careful evaluation and data migration planning.
To choose the right modernization approach, assess the feasibility, cost, and timeline for each option, considering the complexity of the legacy healthcare app, its role in patient care delivery, and the potential impact on clinical workflows.
It’s also important to identify the resources and expertise required for the modernization project, such as knowledge of HIPAA regulations, HL7 standards, and clinical data management for successful execution.
Step 3: Choose the right technology stack
Start by evaluating modern healthcare technologies and cloud platforms like AWS, Google Cloud, or Azure, which offer scalability, interoperability, and robust security features. Consider cloud-based EHR systems, such as Cerner or Epic, which can handle large volumes of patient data and ensure seamless integration with other healthcare systems.
Next, prioritize compliance with healthcare industry regulations and standards. Ensure that the chosen technologies provide HIPAA-compliant data storage and secure communication protocols like HL7 FHIR. We also recommend using the blockchain technology for secure data sharing and auditing.
Finally, align your tech stack with the organization’s long-term goals and budget. Select technologies with proven track records in the healthcare industry and strong community support. For example, if developing a mobile health app, consider cross-platform frameworks like React Native or Flutter, which offer a rich ecosystem of healthcare-specific libraries and tools.
Balancing cost with functionality and future-proofing your IT infrastructure ensures a sustainable and effective modernization effort.
Step 4: Specify integration goals
Defining integration goals aligns the healthcare organization’s IT modernization efforts with its overarching strategic objectives.
The following are common integration goals that healthcare organizations should consider:
- Enabling real-time access to patient data across different departments
- Facilitating secure sharing of medical records with external providers
- Ensuring interoperability between clinical systems and emerging technologies like wearables or remote monitoring devices
- Streamlining administrative processes through integrated billing, scheduling, and inventory management systems
To prioritize the most appropriate goals, consider the following steps:
- Start by evaluating the specific challenges your organization faces with current legacy systems. For instance, if data silos are a significant issue, prioritizing interoperability should be high on your list.
- Given the importance of compliance in healthcare, goals related to meeting regulatory standards and ensuring data security must be prioritized.
- Consider the resources available, including budget, technology, and human expertise.
- Prioritize goals that can be achieved within the current resource constraints.
- Conduct a cost-benefit analysis to determine each integration goal’s feasibility and potential impact, ensuring that the invested resources yield tangible benefits.
Step 5: Choose an integration method and conduct the integration of middleware
When choosing an integration method, consider factors like system compatibility, data security, and scalability. Here’s a table outlining common integration methods, their use cases, and examples:
| Integration Method | Use Cases | Examples |
| Enterprise Service Bus (ESB) | Integrating multiple applications and systems across the healthcare organization, enabling data exchange and orchestration of complex processes. | Integrating EHR with billing, lab, and clinical decision support systems. |
| Point-to-Point Integration (P2P) | Connecting two specific applications or systems directly suitable for simple and straightforward integrations. | Integrating a medical device with an EHR system for seamless data transfer. |
| API Integration | Exposing and consuming APIs to enable data exchange and integration between different systems and applications. | Integrating a telemedicine platform with an EHR system using APIs to access patient data. |
| Robotic Process Automation (RPA) | Automating repetitive tasks and processes, particularly legacy systems with limited integration capabilities. | Automating the transfer of data from legacy systems to modern EHR systems. |
| Integration Platform as a Service (IPaaS) | Providing a cloud-based platform for integrating various applications and systems, enabling rapid integration and reducing the need for on-premises infrastructure. | Integrating cloud-based healthcare applications with on-premises systems, such as EHR and practice management systems. |
To conduct middleware integration effectively, follow these steps:
- Assess your existing systems and identify integration requirements, considering data formats, security protocols, and performance needs.
- Select the appropriate middleware solution based on your requirements and integration methods.
- Define data mappings and transformations to ensure seamless data exchange between systems.
- Implement security measures, such as encryption and access controls, to protect sensitive healthcare data.
- Test the integration thoroughly, simulating various scenarios and data flows to ensure proper functionality.
- Deploy the middleware solution and monitor its performance, addressing any issues.
- Train end-users and support staff to ensure smooth adoption and ongoing maintenance.
- Continuously evaluate and optimize the integration process, adapting to evolving healthcare IT needs and technologies.
Step 6: Develop and test modern system components
To develop and test modern system components effectively, you should:
- Clearly define the requirements and specifications based on input from healthcare professionals, IT experts, and other stakeholders.
- Next, employ an iterative development approach to build and test the components in small, manageable increments.
- Establish cross-functional teams that include developers, quality assurance specialists, and subject matter experts to foster collaboration and continuous improvement.
As the development progresses, incorporate various testing techniques tailored to the healthcare domain.
- Usability testing ensures the system’s user interface is intuitive and easy to navigate for healthcare professionals.
- Conduct user acceptance testing with real healthcare workers to gather valuable feedback and refine the system accordingly.
- Performance testing is equally important, as healthcare IT systems must be able to handle peak workloads and high volumes of data without compromising responsiveness or functionality.
- Load and stress testing can identify potential bottlenecks and help optimize system performance.
- Security testing is a top priority in healthcare due to the sensitive nature of patient data and strict regulations like HIPAA. Assess the system’s security measures, such as data encryption, access controls, and vulnerability management, to protect confidential information.
- Integration testing is also crucial, as modern healthcare IT systems often need to seamlessly integrate with existing systems, such as laboratory information systems, radiology systems, or third-party applications. Verify that data integrity and smooth information exchange are maintained across different systems and departments.
Step 7: Carry out data migration
To carry out data migration in an effective manner:
- Begin by profiling and cleansing your legacy data, identifying and addressing any inconsistencies, duplicates, or errors.
- Next, define the data models and schemas for the modernized system. This involves understanding the new system’s architecture and designing a schema that aligns with stakeholders’ requirements.
- Once the data models are defined, perform the Extract, Transform, and Load (ETL) process to migrate data from the legacy system to the new system. This may involve writing scripts or using specialized tools to automate migration.
- After the migration, validate and reconcile the migrated data. Conduct thorough testing to ensure data integrity, accuracy, and completeness. Reconcile any discrepancies between the legacy and modernized systems and address the issues.
- Throughout the data migration process, maintain open communication with stakeholders, document any challenges or decisions, and continuously monitor the progress.
Step 8: Enforce monitoring and optimization
Monitoring ensures the smooth operation and optimal performance of modernized healthcare IT systems. It enables healthcare organizations to proactively identify and address potential issues before they escalate, minimizing downtime and ensuring the continuity of critical services.
The process of monitoring healthcare systems involves several key steps:
- Define monitoring objectives: Determine the specific aspects of the system that require monitoring, such as application performance, system resources, security events, and compliance requirements.
- Establish monitoring metrics: Identify the key performance indicators (KPIs) and thresholds that trigger alerts or notifications. These metrics may include response times, resource utilization, error rates, and security events.
- Implement monitoring tools: Deploy the appropriate monitoring tools and configure them to collect and analyze the relevant data from various system components, including servers, databases, networks, and applications.
- Set up alerts and notifications: Configure the monitoring tools to generate alerts and notifications when predefined thresholds are breached or anomalies are detected. These alerts can be sent to designated personnel or integrated with incident management systems.
- Analyze and interpret data: Regularly review and analyze the monitoring data to identify patterns, trends, and potential issues. This analysis can provide insights into system performance, resource utilization, and possible bottlenecks.
- Optimize and fine-tune: Based on the insights gained from monitoring data, implement necessary optimizations to improve system performance, efficiency, and security.
Popular monitoring tools for healthcare systems include:
- Splunk: A powerful data analytics platform that can collect, index, and analyze machine data from various sources, including logs, metrics, and events.
- Nagios: An open-source solution offering comprehensive monitoring capabilities for servers, applications, networks, and services.
- Zabbix: An enterprise-class open-source monitoring solution that supports distributed monitoring of various IT components, including servers, networks, and applications.
- SolarWinds: A comprehensive network and system monitoring tool suite that caters to various IT environments, including healthcare.
- AppDynamics: An application performance monitoring tool that provides deep visibility into application performance, user experience, and business transactions.
Modernizing healthcare IT systems is daunting, but some organizations have successfully navigated this journey.
Case studies: Healthcare IT legacy system transformations
Let’s look at some real-world examples of healthcare organizations transforming their legacy systems.
#1. St. Luke’s University Health Network improved staff efficiency by modernizing legacy infrastructure on Azure
St. Luke’s University Health Network provides a range of healthcare services in 300 locations across Pennsylvania and New Jersey.
Challenges
St. Luke’s legacy access center systems made it difficult to track patient interactions across calls and departments. Without a centralized view, staff had to manually search for patient details while on the phone–slowing response times and affecting service quality. The organization needed to modernize its infrastructure, connect disparate systems, and implement a unified CRM solution to deliver faster, more personalized support across the patient journey.
Solutions
St. Luke’s used Microsoft FastTrack to accelerate cloud adoption. It deployed Microsoft Dynamics 365 across its access centers for case tracking, appointment scheduling, and real-time updates to electronic health records (EHR). Using Microsoft Cloud for Healthcare, the team integrated data from Epic, enabling a 360-degree patient view within the CRM system. St. Luke’s also leveraged Twilio for personalized call experiences and Power BI to enhance analytics and monitor referral conversions.
Key results
- Enabled one-click appointment scheduling and patient notifications
- Unified CRM and health record systems to simplify patient support
- Reduced time spent searching for information, improving staff efficiency
- Improved analytics to track case outcomes and drive better engagement
#2. Fairview Health Services modernized legacy apps and saved $3M by adopting cloud-based endpoint management
Fairview Health Services is a nonprofit healthcare organization operating hospitals and clinics across Minnesota.
Challenges
Fairview was working with legacy applications, processes, policies and governance models that were difficult to scale and secure. While Microsoft 365 had already helped modernize parts of its technology stack, the organization wanted to fully transition to a modern, secure experience by deploying Windows 11 Enterprise and adopting cloud-based endpoint management. The goal was to reduce complexity, improve compliance, and unlock the full value of its existing Microsoft entitlements.
Solutions
Fairview adopted a cloud-based endpoint management model by shifting from traditional device management to Microsoft Intune. This enabled streamlined, centralized management of its digital infrastructure, enhancing security, simplifying compliance, and reducing operational overhead. By leveraging in-place upgrades and automating deployment, Fairview modernized its endpoint environment with minimal disruption to clinicians and staff.
Key Results
- Upgraded over 80% of its 34,000-device fleet via in-place upgrades
- Reduced deployment costs by over $3 million compared to past migrations
- Strengthened security and compliance posture
- Minimized disruption for end users during modernization
While healthcare organizations have demonstrated the benefits of modernizing their IT systems, the journey to modernization has its challenges.
Challenges of modernizing legacy systems in healthcare
Modernizing healthcare systems is a complex undertaking that involves a wide range of stakeholders, including healthcare providers, patients, payers, and government agencies. The process of modernization requires significant changes to existing infrastructure, processes, and mindsets, which can present the following challenges.
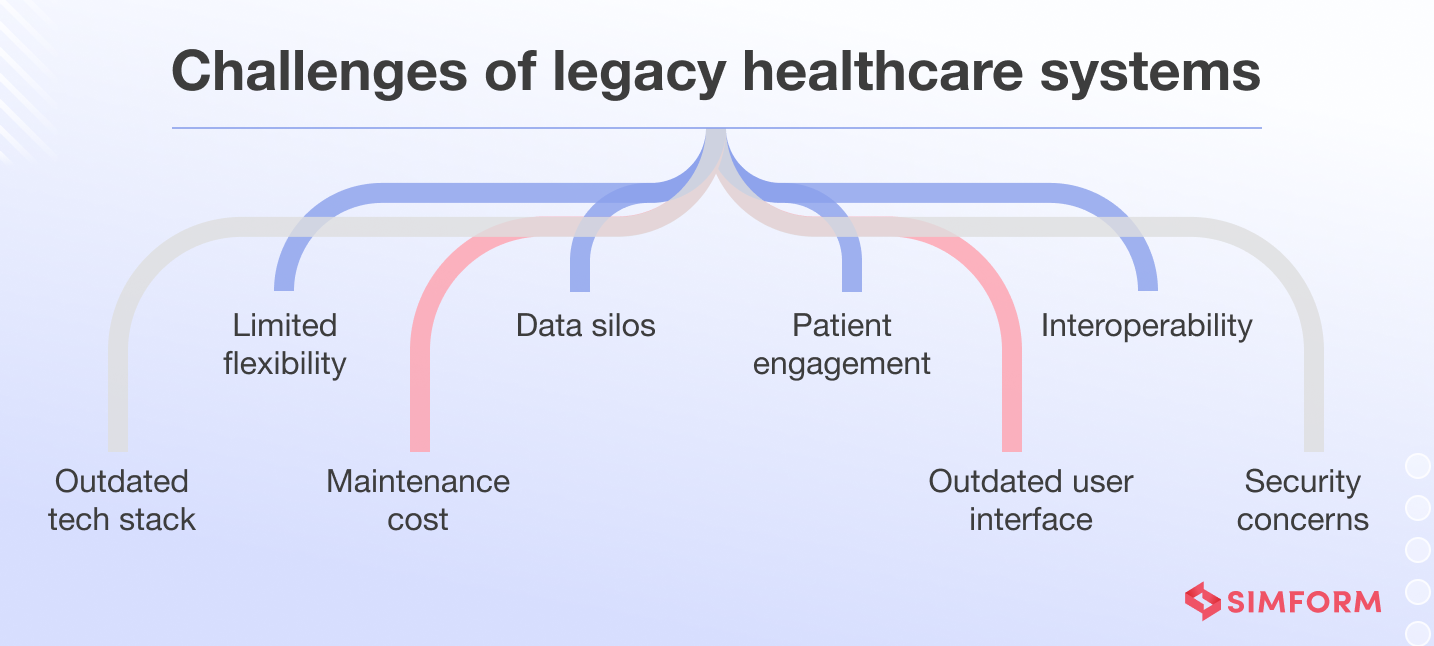
#1. Integrating new technologies with existing systems
One of the primary challenges in modernizing legacy systems is the integration of new technologies with existing systems. Legacy systems often rely on outdated architectures and programming languages, making it challenging to integrate them with modern software and hardware solutions seamlessly. This compatibility issue can lead to interoperability problems, data silos, and inefficient workflows, ultimately hindering the desired benefits of modernization.
#2. Data migration and integrity
Healthcare firms possess a wealth of patient data accumulated over years of operation. Migrating this vast amount of data from legacy systems to new platforms poses a significant challenge. Ensuring data accuracy, completeness, and integrity during the migration is crucial, as any errors or data loss could compromise patient care and potentially lead to legal liabilities.
#3. Regulatory compliance and data security
The healthcare industry in the United States is subject to stringent regulations and data privacy laws, such as the HIPAA (Health Insurance Portability and Accountability Act). Modernizing legacy systems necessitates compliance with these regulations, from data migration to system implementation and ongoing maintenance. Failure to adhere to regulatory requirements can result in severe financial penalties and reputational damage.
#4. Change management and user adoption
Introducing new systems and processes requires more support from healthcare professionals accustomed to established workflows. Change management and user adoption are critical challenges that require practical training, communication, and stakeholder engagement. Healthcare organizations must invest in comprehensive training programs and ensure end-users are comfortable and proficient with them.
#5. Cost and resource constraints
Modernizing legacy systems is a resource-intensive endeavor, both in terms of financial investment and human capital. Healthcare organizations often operate under tight budgets and may struggle to allocate sufficient funds for system upgrades, infrastructure improvements, and staff training. Additionally, securing skilled IT professionals with expertise in legacy systems and modern technologies can be challenging, further exacerbating resource constraints.
#6. Business continuity and downtime management
Healthcare operations are time-sensitive and critical, making system downtime a significant risk. During the modernization process, healthcare organizations must ensure business continuity by carefully planning and executing system transitions, minimizing disruptions to patient care, and implementing robust backup and disaster recovery strategies.
#7. Legacy system documentation and knowledge transfer
Legacy systems often lack comprehensive documentation, and the knowledge of their intricacies may reside with a few individuals nearing retirement. Capturing and transferring this institutional knowledge to the modernization teams is a complex challenge that requires proactive knowledge management strategies.
How can Simform help you modernize your legacy healthcare systems?
Modernizing legacy healthcare systems is a complex task. It demands expertise to navigate the intricacies of outdated infrastructures, especially with stringent regulations like HIPAA.
As a Microsoft Solutions Partner for Digital & App Innovation, Data & AI, Infrastructure, and Security, Simform is uniquely positioned to help healthcare organizations modernize their IT landscape using Microsoft Azure’s powerful cloud ecosystem.
Here’s what Simform’s healthcare IT system modernization comprises:
- Comprehensive assessment of legacy healthcare systems
- Identify critical pain points and inefficiencies
- Develop a tailored modernization roadmap
- Migration of legacy workloads to the cloud with minimal disruption
- Implement secure, scalable cloud infrastructure on Azure
- Integrate advanced healthcare analytics and AI solutions
- Ensure compliance with healthcare regulations
- Migrate legacy data to modern data lakes or warehouses
- Enhance interoperability between disparate systems
- Implement robust disaster recovery and data backup solutions
- Train healthcare staff on new systems and processes
- Continuously monitor and optimize system performance
- Provide ongoing support and maintenance services
- Enable seamless patient data access and exchange
- Implement telehealth and remote patient monitoring capabilities
- Improve patient engagement through mobile apps and portals
Partner with Simform to modernize your healthcare systems and unlock the full potential of digital transformation in healthcare.